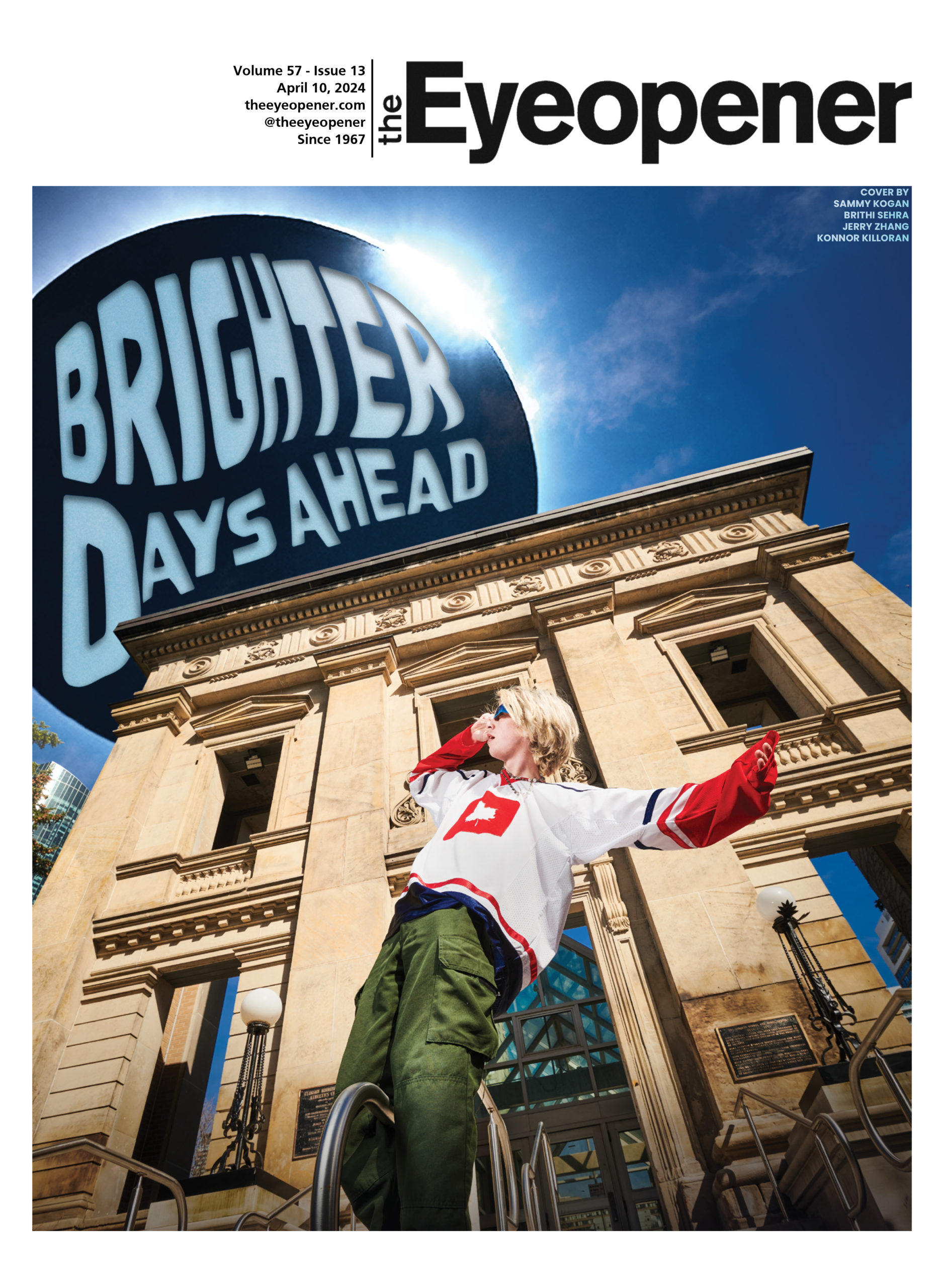
Words by Rowan Flood
Visuals by Sammy Kogan & Kinza Zafar
Trigger warning: This story contains mentions of overdose, drug poisonings, sexual violence and death
“I have a personal story,” says Brais Baliñas abruptly.
Around 13 people are gathered at a friend’s party. He’s been watching a friend who has been drinking but, at the moment, seems “perfectly fine.” Suddenly, he’s asleep on a chair with his head slumped onto his chest. And then he pukes. Baliñas fears his friend might choke and adjusts his position. He cleans him up. But what now—call his parents? No, says the friend. Put him in an Uber? No, he might puke again. The subway then. Baliñas drags him to the subway. He stands with his wobbling friend at Spadina Station with a metal bowl and trash bag in hand.
Baliñas, a fourth-year nursing student, and the friend got home safely. But what if they hadn’t? What if his friend had taken another substance and was overdosing? You’ve probably witnessed friends being very drunk to the point where they throw up or lose the ability to speak—this is a form of overdosing. In an emailed statement to The Eyeopener, Toronto Public Health (TPH) said that an overdose or poisoning can occur when someone consumes “a toxic, excessive or lethal amount of a drug or medicine into their body that can result in adverse and potentially life-threatening effects.” Throwing up and being unable to speak are adverse effects.
In B.C., a 10 to 18-year-old is more likely to die from a toxic drug overdose than anything else. The Government of Alberta’s substance use surveillance system report states they lost 100 people aged 20 to 24 to drug poisoning deaths in 2022. In Ont., from 2014 to 2019, rates of opioid-related deaths tripled for people ages 15 to 24, according to a report from the Ontario Drug Policy Research Network at Unity Health Toronto. The immense loss is nationwide and it’s not stopping.
In 2021, the Toronto Paramedic Services received over 6,000 non-fatal suspected overdose calls and 357 fatal ones. An overdose can also be referred to as drug poisoning, which, more accurately, reflects what is biochemically happening in the body. It’s when someone’s central nervous system is overwhelmed by consuming too much of a substance or combination of substances, explains Casey Schapel, harm reduction lead at Casey House, a specialty Toronto hospital.
When considering the amount of overdoses, understanding what drugs are out there is part of understanding the entire picture. For example, if you purchase a bag of cocaine off a street corner, you may not be completely sure what it contains. Toronto’s Drug Checking Service takes drug samples every other week to compile data and provide relevant information. From Sept. 23 to Oct. 6, they tested 123 drug samples, 39 per cent of which was the expected drug of fentanyl. According to the service, the “expected drug” is what you believe the drug is when acquired but unexpected drugs can be found.
Safer opioid supply programs have emerged across Canada and in Toronto in response. The programs have various goals, including lessening the dependency on an unregulated drug market and reducing the risks of overdose and the harms of substance use, outlines the Centre on Drug Policy Evaluation. This is harm reduction.
Schapel explains harm reduction is partly a philosophy that accepts that substance use occurs whether legalized or not. Harm reduction is treating substance use as part of holistic healthcare and it means working with people based on their own goals, whether it be abstinence from drugs or reducing drug-associated risks, he says. A ‘drug-associated risk’ can be anything from risks to people’s health to the negative impacts that come with drug criminalization. Decriminalizing drugs can help reduce barriers and stigma that prevent people from receiving help, according to a Government of British Columbia’s webpage.
Simply put, Felicia Langdon, the 2SLGBTQ+ provincial youth outreach worker at the mental health agency Lumenus, believes that harm reduction “is anything that you can do to reduce harm.”
The nationwide problem doesn’t end at a university in the middle of Canada’s largest city surrounded by some of the country’s best hospitals—Toronto Metropolitan University (TMU) is part of the story.
Students must be educated to make safe choices and understand the world surrounding them. Some students may not know what the life-saving medicine naloxone—a medication that reverses the symptoms of an opioid overdose by blocking the effects of opioids in the brain—is, explains TPH. Or what the building on campus they may feel unsafe around—The Works, just across the Victoria Street Tim Hortons—even does.
It’s around 6:30 p.m. Reza Zareian’s physics lab just ended. Snow is falling around the ivy-covered bricks of Kerr Hall. The mound of grass surrounded by sparse trees in the centre of the square-shaped buildings holds a girl struggling to walk.
“I can’t breathe properly,” she says through loud laughter. She adds that she can’t find her way home, so Zareian calls campus security, believing she’s taken substances. He had to leave, but his friends later told him that after campus security came, an ambulance followed.
Zareian is a second-year biology student who rarely drinks except during the occasional party. He has never been in such a situation but dealt with it as best he knew how.
Sarah Hick, on the other hand, has been in many situations with people who use drugs. Hick, an outgoing fourth-year nursing student who works in healthcare, always has a naloxone kit in her backpack. She finds her words quickly as she speaks about her passion for nursing.
She has witnessed substance use and its impact “right out of the gate.” She’s learned the importance of not viewing substance use as something connected to someone’s moral character and remembers that someone “can be an asshole and have literally never touched drugs.” Her hands move rapidly to reinforce her opinions, yet she continues to laugh and smile every other sentence.
At Casey House, where Hick completed a placement in her third year, everyone is familiar with harm reduction. Still, she understands that someone from a different background may have no idea what naloxone is or the reasoning behind providing clean needles.
Picture a child growing up in a suburban neighbourhood in North York, Toronto, with parents who are bankers. Maybe they don’t discuss mental health, sex or drugs much at home and have no visible unhoused people in their area or any nearby drug consumption sites. Soon, the child is commuting to TMU in downtown. Immediately, they are exposed to people and places that might be uncomfortable to them. Hick recognizes that people who use drugs can sometimes appear agitated, which can be intimidating, but she clarifies that it does not make them undeserving of respect and care. Nevertheless, people have to be educated about it.
Many people hang out outside The Works on Victoria Street, a supervised consumption site on campus. Occasionally, someone may yell or appear unwell, but folks just exist in the space.
Zareian commutes to school from North York, and when he gets off the subway, he feels unsafe passing by The Works. He describes noticing “aggressive” stares but does not know what happens inside the building.
TPH explains through an email to The Eyeopener that The Works services “include providing harm reduction supplies and counselling, supervised consumption services, injectable opioid antagonist therapy (iOAT), naloxone training and mobile and community outreach.”
The Works is not that disconnected from the university. They say they’ve engaged with the school several times through overdose response training, student tours and outreach projects. They believe through this engagement, there has been an increased understanding of drug use and less stigma.
TPH explains in the email that by “speaking openly about the impacts of substance use, we can better address the stigma and discrimination that present a major barrier for people who use drugs to access the services they [need].”
If TMU says ‘this is The Works, this is what they do and you may walk past people using substances. If you want to talk to somebody there or if you’re curious, we can provide education and resources,’ then it would be beneficial for the students, says Hick through a rising voice.
Hick acknowledges that Toronto is a city where many people struggle with housing insecurity, mental health and substance use. Therefore, naturally, people visibly facing such challenges will be seen in public.
“It’s not your space, it’s Toronto,” says Hick.
Connecting, supporting and educating youth on substance use is possible. Schapel approached his work with youth in two ways: first, with preventative education through information sessions. Youth were taught about the different kinds of substances, what they do and their risks so they could make informed decisions on how to engage with substance use if they choose to. They were educated on the various resources available for accessing support if it became an issue for them. Second, there was a youth needle exchange program, drop-in counselling and health consults with nurses. Schapel emphasizes that making services to youth “low-barrier” is at the core of their success.
“For a lot of young people, engaging in health care for the first time can be quite stigmatizing,” says Schapel.
Langdon describes how the stigma that youth can experience comes from people thinking that young people don’t know what’s best for them or what they need, leading them to feel like they lack autonomy.
Many youths may recieve health care in university for the first time as independent people. Schapel says there can be an assumption that young people don’t engage in substance use or experience social challenges.
“It’s really about finding out what young people feel they need,” he says. Being able to tailor services and education to specific people based on their needs is necessary. Students may have trauma histories, be from marginalized populations or experienced hate crimes and systemic oppression.
Many students no longer have access to a familiar family doctor or local walk-in clinic. Schapel explains that hosting groups to provide information, overdose education and naloxone kits that incorporate food, hygiene supplies and access to transport or clothes is a low-barrier way to engage in a safe environment. Schapel attests that actions like these open up conversations about substance use when the person feels ready. Youth will realize the faces that become familiar as they engage through low-barrier services also become safe people to talk to when things get unmanageable. All in all, the more informed a choice a young person can make about their substance use, the better for them.
“It’s about empowering young people,” declares Schapel.
The organization Langdon works with, Lumenus, provides a wide range of mental health and developmental services, including a youth harm reduction program. She agrees that tailoring a low-barrier harm reduction approach to the individual is critical. She explains that youth can discover their version of harm reduction through a “less clinical” method of art and music.
Another less clinical method of engaging students in harm reduction is a dildo ring toss or a lube taste test, says Sam DeFranco, the support coordinator for The Centre for Safer Sex & Sexual Violence Support at TMU. Despite the seriousness of her role, her eyes brighten as she speaks of her work. She agrees that educating students through “cool” games and community activities is instrumental—students get enough “boring” lectures in class. The goal is to get students more comfortable talking about the uncomfortable. “Have a sex toy!” She exclaims mid-sentence.
Fun is part of it but she also recognizes that to help students trust the support TMU offers, removing the stigma and creating safety is essential. If a student approaches her saying they’ve been using drugs and it’s starting to impact their school, she’s empathetic.
Some faculty who have grown up with the stigma may talk about drugs and sex in “hushed voices.” DeFranco tells them, “That’s really hard; it must be really difficult to be having those issues with drugs.”
DeFranco again emphasizes that in some situations where students are using substances, abstinence isn’t always the best solution. She will help students decide what they want and then determine the tools to get them there.
Another layer of harm that comes with substance use is sexual violence. DeFranco explains that much sexual violence happens when someone is intoxicated. Even further, sexual violence happens more to people from minority groups. Systemic patterns and problems are all related and any conversation on equity has to involve a host of issues, says DeFranco.
DeFranco believes the university has a responsibility to students regarding substance use. She explains that students feel many pressures because of university-life and that “theoretically,” the university should be on the students’ side. However, she thinks TMU often sees itself as a business. Perhaps when the school offers workshops on increasing job skills, they could provide naloxone training, which, as DeFranco points out, is a good job skill.
The university must also realize who its student body is: one that, during the pandemic, faced educational disruption and “learning losses,” says the Ontario COVID-19 Science Advisory Table in a 2021 report.
Academic education is one thing, but what about sex and drug education? The Grade 9 to 12 curriculum in Ontario does mention education about safe sex practices such as condoms, but DeFranco has found that since the pandemic, students are less knowledgeable about sex. A new curriculum in 2015 was reverted by Doug Ford in 2018 to the 1998 version, which limits topics on social media and 2SLGBTQ+ communities. People have approached her booth and asked, “What’s this?” to a condom…If students find a condom unfamiliar, what would they think of a naloxone kit or a needle drop box?

Hick urges students to learn to use and carry naloxone kits. She describes how simple it is to use and to access—you could walk into a Shoppers Drug Mart and pick one up for free. Part of her insistence on naloxone comes from the fact that she’s aware that students party and do drugs. She’s also aware that many probably aren’t thinking about testing their drugs or having a plan in case someone overdoses.
Hick brings up another belief that many young people may have: their use of drugs and alcohol completely contrasts with how others use drugs. Sure, Hick says a student might be at a $20-cover club, wearing a clean dress and getting bottle service—but they’re still consuming substances, just as someone on the street may be. If a friend says, ‘I was blackout drunk last night and it was crazy,’ you might respond with, ‘haha, tell me what happened.’ But if they say, ‘I overdosed last night,’ there would be a different response. To be clear, blacking out from drinking or greening out from cannabis use means you have taken too much of a substance—thus going ‘over’ your intended ‘dose.’
Hick recognizes that the work the university does for mental health, such as therapy dog sessions and workshops on healthy relationships and safer substance use, is not the end of supporting students.
Students put their trust in the institution they attend. They hope their money goes towards a good education, resources, equipment and facilities. A university is a place for learning and many students look up to their educators, who could provide tools and education about harm reduction if prioritized.
TMU has offered opportunities for students to engage in harm reduction and substance education, but how many students can use a naloxone kit or explain what harm reduction means? Having naloxone kits available to students at TMU is something that many harm reduction and student support workers believe is essential.
Langdon states, “Naloxone is something that can save a life, can change a life…You could be at a party, you could be hanging out with friends, you literally could be doing anything,” and carrying naloxone could prevent another loss.
TMU uniform security guards are trained to use naloxone and started carrying it in May 2018, says the school’s Community Safety and Security department through an emailed statement to The Eye.
When asked about naloxone availability on campus, TMU Student Wellbeing’s answers only mentioning its accessible use for campus security staff.
Having people on campus who know how to administer naloxone is crucial if there is an incident, but students have lives outside of university, too, expresses Langdon. Student Wellbeing says they “strive” to create an environment where students are informed and feel safe around substances. Along with several university associations, Student Wellbeing launched Substances and TM(U). The campaign aimed to open conversation for students on substance use and their relationship to substances.
The Works believes their location on campus has allowed students to learn about the struggles that come with drug use, but in the next twenty-four months, they will be relocated.
TPH explains via email that, “CreateTO, in partnership with TPH leadership and their partners, will continue to support the relocation of these critical services over the next two years to ensure continuity of care and minimize the impact on residents and TPH clients.”
As previously reported by The Eye, TMU recently acquired the Victoria Street building and it may soon be converted to offer additional office or research space.
You go to the right of a community centre in Toronto and open a door. When you enter, a big table and a bunch of old brown leather couches surround the room. There is a rug. Yet there are also gloves and sharp disposable bins. There are nurses and cubicles. Free clean needles and alcohol swabs are handy. There is another room with a vital machine, oxygen and a defibrillator.
“You could chill there,” says Baliñas, “Just go through your high in that safe space.”
You’ve entered the safe consumption site that Baliñas, who once guided his drunk friend home, visited last year. The site is designed to prevent the risks of infection, overdose and police. Places like this exist, where every safety net is ready, and Baliñas is in awe as he walks through.









Leave a Reply