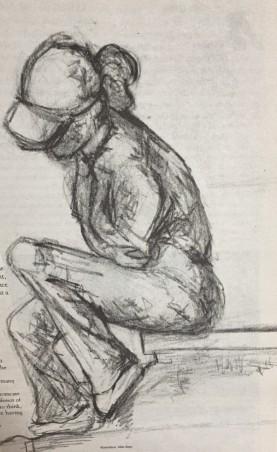
Nearly one in five Canadian university students will suffer from mental illness, including severe depression and schizophrenia, so why isn’t anyone talking about it?
By Siri Agrell
The mass of men lead lives of quiet desperation
-Henry David Thoreau
We have all watched it happen. The smiles of friends, classmates or family members fade into rigid masks while conversations taper into silence. We have seen people grow distant, withdrawing into the darkness of what ever is bothering them, assuming they will once again emerge. But for many, this marked sadness, confusion and desperation is not just a mood but a clinical disorder experienced by nearly one million Canadians.
Their diagnoses range from depression, schizophrenia and anxiety, to obsessive-compulsive disorders and psychosis. One in five Canadians will experience a form of mental illness serious enough to impair their ability to function within society. The most common mental illness is depression, a state of extreme sadness, despair, hopelessness, and low self-esteem. Depression is often accompanied by physical symptoms such as a loss of appetite and decreased energy. These negative moods can be triggered by a traumatic event, but the cause of depression is a chemical imbalance in the brain’s neurotransmitters. Low levels of these chemicals prevent the brain from transmitting signals normally. This creates chaos in the parts of the brain that control appetite, concentration, mood, sleep, and libido.
But despite the physical causes and devastating effects of depression, many people’s suffering goes unnoticed or unaddressed.
“Depression is hard to spot because it’s one of those things where the symptoms are common to other things — being tired, feeling sad,” says Carol Stuart, professor of child and youth care. “Even the cognitive problems like not being able to think, people assume they’re just not getting it when actually their minds are having problems processing information.”
Stuart says that mental illness can be especially hard to spot, diagnose and treat among university students whose moods are naturally prone to swings according to romantic, academic or other personal concerns. Symptoms that are associated with mental health disorders are easily confused with symptoms of a busy, stressed-out and exhausted university student. But in fact, many people face their first experiences of mental illness in between the ages of 18 and 25. To improve the odds of diagnosing and treating these students, Stuart says people’s general awareness and acceptance of the issue has to improve.
“It has to be seen just like any other illness,” she says. “But there’s a real stigma about admitting you have a problem and going to get help.”
The most important thing people can do, notes Stuart, is to accept that mental illness occurs all around us, and must be acknowledged.
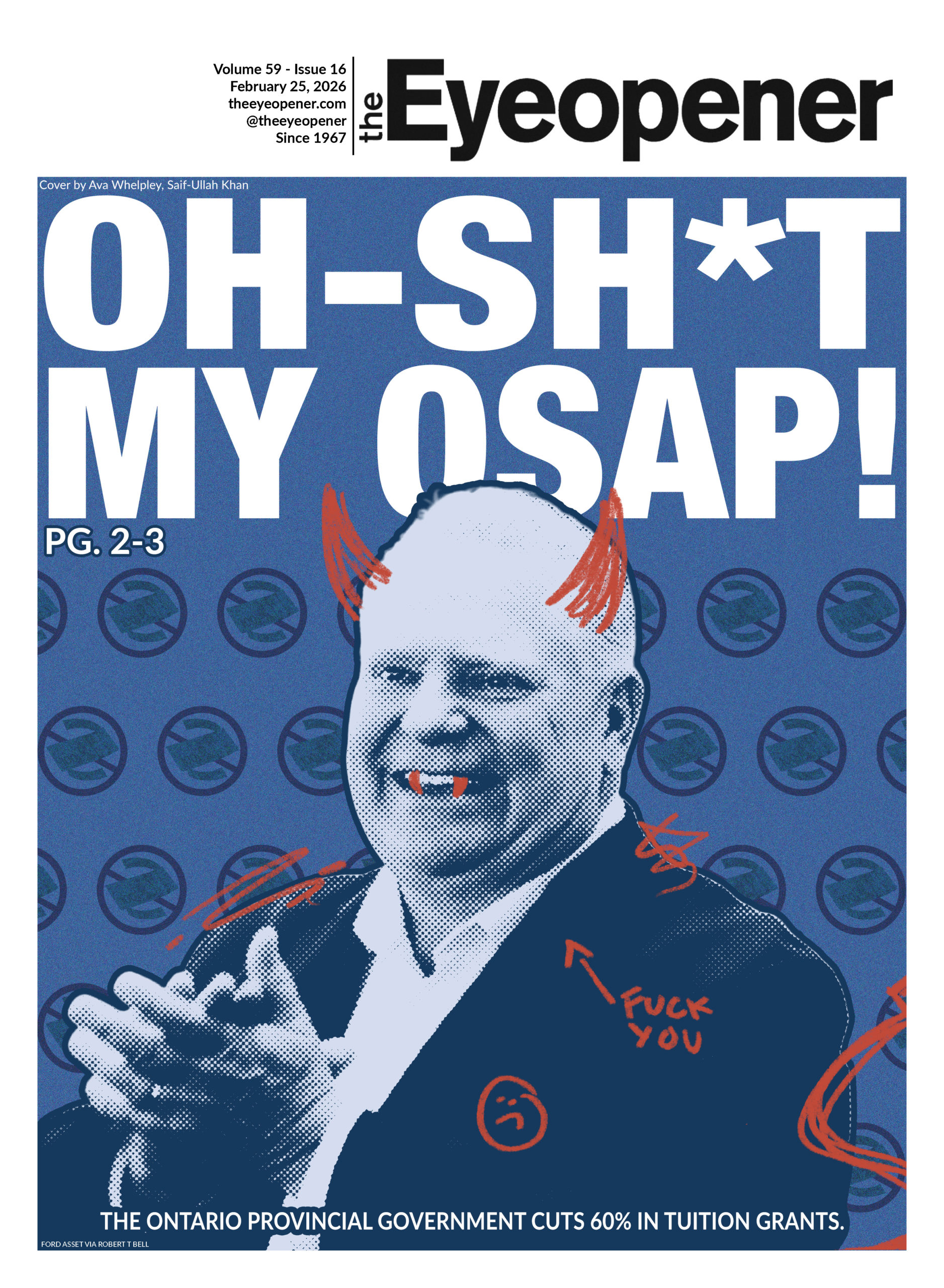
“We need public discourse and very specific crisis intervention tools,” she says. “We hold seminars on how to get an OSAP loan, why not have open forum on how to recognize the signs and symptoms of depression so that people know how to help.”
Dr. Ester Cole, a Toronto psychologist, says there are several key symptoms to look out for if you’re concerned a friend may be going through a mental health crisis. She says that while it’s hard to differentiate between the normal problems of young adults, there are several important indicators, including the longevity of stress and anxiety.
“It can start with having an exam, but then it stays and it doesn’t go away,” says Cole.
People suffering from depression will also pull away from friends and family and avoid doing things that used to be fun. “Their emotions might have changed,” says Cole. “They’re self-critical and more pessimistic.”
While Cole says it’s normal for students to feel stressed with the weight of school and other pressures, it’s up to the medical professional to diagnose the severity of that anxiety, so concerned students should seek out their advice. Apart from lifestyle changes, doctors will assess the individual’s physical changes that can range from insomnia to staying in bed all day and from eating a lot to not at all.
“We ask how similar or different it is from the way they usually are,” says Cole.
Both Cole and Stuart agree that paying attention to the changing moods of those around you, and to the fluxuations in your own moods, is the most important step towards addressing mental illness. “Everyone wants to say ‘It’s going to be okay, I’ll solider on’,” says Stuart. “But we can’t do that anymore, we have to start taking action.
With files from Emily Bowers and Caitlin Martella









Leave a Reply